Definition of a Broken Femur
A broken femur, or a fracture in the thigh bone, is a serious injury that is often the consequence of high-impact incidents such as car accidents. These fractures are among the most severe injuries that can affect the leg, often requiring immediate medical intervention, including surgery, and extensive physical therapy for full recovery. The complex nature of a femur fracture can lead to a cascade of related health problems and long-term disabilities, particularly if not treated promptly and properly.
As an attorney who specializes in representing clients with broken femurs, I recognize the complexity of these cases. They often require a multifaceted approach that goes beyond the mere legalities. Understanding the medical aspects, negotiating with insurance companies, dealing with medical providers, and fighting for fair compensation all contribute to the intricate nature of these cases. Additionally, the emotional toll that such a severe injury can take on the victim and their family further compounds the challenges.
A broken femur can drastically alter a person’s quality of life, not only due to the immediate pain and suffering but also in the long term as they deal with potential lifelong disabilities. This may affect their ability to work, engage in hobbies, or even perform everyday tasks. The potential loss of income and mounting medical bills adds financial stress to an already overwhelming situation.
In these cases, legal representation is not merely about pursuing compensation. It is about providing support, guidance, and advocacy to ensure that the victim’s rights are upheld at every stage of the recovery and legal process. Ensuring that clients receive the necessary medical care, rehabilitation services, and support to return to as normal a life as possible is the ultimate goal. This requires not only legal expertise but also empathy, understanding, and a commitment to fighting for what is right for the individual and their family.
The path to recovery from a broken femur is often long and filled with challenges, and the legal journey is no less complex. But with the right legal guidance, victims can navigate this difficult time with confidence, knowing that their needs and rights are being prioritized.
Prevalence of Broken Femur Injuries
The femur, or the thigh bone, is the largest and one of the strongest bones in the human body. Broken femur injuries, also known as femur fractures, are significant health concerns that can be both painful and debilitating. Understanding the prevalence of these injuries is essential for healthcare planning, injury prevention, and rehabilitation strategies.
Types of Femur Fractures
Femur fractures can be broadly categorized into three types:
- Proximal Femur Fractures: These fractures occur near the hip joint and include hip fractures.
- Femoral Shaft Fractures: These involve the main portion of the bone.
- Distal Femur Fractures: These fractures happen near the knee joint.
Risk Factors
Several factors contribute to the risk of femur fractures, including:
- Age: Older adults are more prone due to osteoporosis.
- High-Impact Activities: Athletes or those involved in physically demanding activities are at a higher risk.
- Medical Conditions: Conditions that weaken bone, such as cancer or metabolic disorders.
- Trauma: Car accidents, falls, or other traumatic events can lead to fractures.
Demographics and Prevalence
- Global Prevalence: Varies across different regions and can be affected by lifestyle, access to healthcare, and community safety measures.
- Age Groups: More common in the elderly but also prevalent among young adults, especially those engaged in sports.
- Gender Differences: May vary between males and females depending on factors such as bone density and activity levels.
Treatment and Rehabilitation
- Surgery: Often required to realign the bone and may involve the use of rods, plates, or screws.
- Physical Therapy: Essential for restoring function and strength.
- Pain Management: May include medications, rest, and supportive measures.
- Long-Term Care: Some patients may require extended care and rehabilitation.
Prevention Strategies
- Education: Awareness of the risk factors and safe practices.
- Physical Fitness: Regular exercise to maintain bone health.
- Environmental Modifications: Addressing potential hazards at home or in public spaces to prevent falls and injuries.
Broken femur injuries are complex and can have long-lasting effects on an individual’s quality of life. Understanding the prevalence and factors influencing these injuries helps in the development of targeted prevention and treatment strategies. Ongoing research and collaboration among healthcare professionals, policymakers, and community leaders are essential for reducing the incidence and impact of these serious injuries.
Understanding the Injury: Broken Femur
Anatomy of the Femur
Function
- Support: As the largest bone in the human body, the femur plays a crucial role in supporting the body’s weight.
- Movement: It facilitates movement by connecting the hip joint to the knee, enabling walking, running, and jumping.
- Protection: Encases and protects the marrow, a critical site for blood cell production.
Structure
- Proximal End: The upper part includes the head, neck, and greater and lesser trochanters, connecting to the hip.
- Shaft: The long, cylindrical part of the femur, strong and straight.
- Distal End: The lower end forms the knee joint with the tibia and patella.
Types of Femur Fractures
Simple
- A fracture where the bone breaks but does not penetrate the skin.
Compound
- Also known as an open fracture, where the bone breaks and protrudes through the skin, increasing infection risk.
Comminuted
- A fracture in which the bone shatters into multiple fragments, often requiring surgical intervention.
Stress Fracture
- A hairline crack in the bone, usually caused by repetitive force or overuse.
Causes and Mechanisms in Car Accidents
- Speeding: Higher speeds increase the severity of injuries, including femur fractures.
- Impact Angle: The angle at which a collision occurs can directly affect the types of injuries.
- Seatbelt Use: Improper use or failure to use seatbelts may increase the risk of serious injuries.
- Vehicle Safety Features: Absence of proper safety mechanisms like airbags can contribute to fractures.
- Road Conditions: Slippery or uneven roads can lead to accidents causing fractures.
Initial Symptoms and Diagnosis
- Symptoms: Pain, swelling, deformity, and inability to move the affected limb.
- Physical Examination: Includes visual inspection and palpation.
- Imaging: X-rays, CT scans, or MRI may be used to visualize the fracture.
- Diagnosis: Combining medical history, symptoms, physical examination, and imaging to determine the type and severity of the fracture.
Potential Complications
- Infection: Especially in the case of compound fractures.
- Blood Clots: Immobility may lead to the formation of clots.
- Delayed Union or Nonunion: Slow or failed healing of the bone.
- Nerve or Vascular Damage: Especially with displaced or comminuted fractures.
- Chronic Pain: Can result from improper healing or associated soft tissue damage.
Understanding the intricate details of the femur’s anatomy, various types of femur fractures, and the potential causes and mechanisms in car accidents helps in both prevention and management. Early recognition of symptoms, prompt diagnosis, and awareness of potential complications are essential for effective treatment and recovery. Collaborative efforts between healthcare providers, traffic authorities, and the general public are vital in reducing the prevalence and impact of femur fractures, particularly those stemming from car accidents.
Immediate Aftermath of the Accident
Immediate First Aid for a Broken Femur
Immediate first aid following a car accident that has resulted in a broken femur is essential to minimize further damage and alleviate pain. Here’s a breakdown of the immediate actions:
Call Emergency Services
- Dial the emergency number in your country (such as 911 in the United States) without delay.
- Provide detailed information about the location and nature of the injuries to ensure appropriate medical help is dispatched.
- Follow the instructions given by the emergency operator.
Assess the Situation
- Ensure your safety and that of others at the scene before attending to the injured person.
- If you’re not trained in first aid, provide support and comfort but avoid moving the injured person unnecessarily.
Comfort the Victim
- Calm the victim and encourage them to remain still.
- Offer reassurance and stay with them until professional help arrives.
Immobilize the Injured Limb
- Immobilization helps to prevent further injury and reduce pain.
- If possible, use items like jackets, blankets, or boards to support the limb without moving it.
- Avoid trying to realign the limb or pushing any protruding bones back into place, as this can cause more damage.
Monitor the Victim’s Condition
- Keep an eye on the victim’s breathing, consciousness, and any other injuries.
- Communicate any changes to emergency responders when they arrive.
Control Bleeding if Present
- If there is visible bleeding, apply gentle pressure with a clean cloth or bandage if available.
- Avoid pressing directly on the fracture site, especially if it’s an open (compound) fracture.
Protect Yourself and Others
- Use personal protective equipment such as gloves if available.
- Direct traffic or use hazard lights if needed to prevent additional accidents.
The immediate aftermath of a car accident involving a broken femur is a critical time. The right first aid actions can make a significant difference in the outcome of the injury. Professional medical care is essential, so calling emergency services must be the priority. Comforting the victim and immobilizing the injured limb can further minimize harm. It’s always beneficial to have basic first aid knowledge, but in the absence of training, following the guidance of emergency dispatchers and awaiting professional medical help is the safest course of action.
Emergency Services Intervention
Prompt intervention by emergency services ensures proper care and transportation to the hospital.
Hospital Admission
Upon admission, immediate assessment and pain management are undertaken to stabilize the patient.
Pain Management
Medication
Pain Management with Medication for a Femur Fracture
Pain management for a broken femur begins at the accident scene and continues throughout the hospital stay, surgery, and rehabilitation. Utilizing medication, such as analgesics, is central to this process, and it involves several aspects:
Immediate Relief at the Scene
- First responders may administer pain relief medications, such as nitrous oxide, to provide immediate comfort.
Hospital Admission and Preoperative Care
- Upon arrival at the hospital, medical professionals will assess the level of pain and may administer a variety of analgesics.
- Non-opioid analgesics, such as acetaminophen or NSAIDs, may be used for milder pain.
- Opioid analgesics, like morphine or hydrocodone, may be employed for more severe pain.
- These medications can be administered orally, intravenously, or through injections, depending on the severity of the pain and the patient’s condition.
Postoperative Pain Management
- After surgery to repair the fracture, pain management becomes even more critical.
- A combination of opioid and non-opioid analgesics may be used to provide balanced pain relief.
- Patient-controlled analgesia (PCA) pumps may also be used, allowing the patient to self-administer a controlled amount of pain medication.
Chronic Pain Consideration
- If pain persists after the initial healing phase, longer-term pain management strategies may be needed.
- This may include extended-release formulations of pain relievers or adjunct medications like nerve pain medications.
Monitoring and Side Effect Management
- Pain medication, especially opioids, must be monitored closely for side effects, including nausea, constipation, and potential addiction or dependence.
- Additional medications may be prescribed to mitigate these side effects.
Patient Education and Collaboration
- Health care providers must educate patients about the proper use of pain medication, potential risks, and the importance of communication regarding pain levels.
- A multidisciplinary approach involving physicians, nurses, pharmacists, and other healthcare providers ensures that pain management is tailored to the individual patient’s needs and preferences.
Pain management using medication, such as analgesics, is a complex and vital aspect of care for a broken femur. It requires careful assessment, a combination of medications, close monitoring, patient education, and collaboration among healthcare professionals. The goal is not only to alleviate pain but to support overall recovery and healing, always considering the individual needs and safety of the patient.
Additional Pain Management Techniques: Ice Application and Elevation
Pain management following a femur fracture is not limited to medications alone. Various complementary techniques can be employed to enhance comfort and aid in recovery. Two such techniques are ice application and elevation:
Ice Application
- Purpose: Applying ice or cold packs helps to reduce swelling and inflammation around the injury site, providing relief from pain.
- Method:
- Use a cold pack or a bag of ice wrapped in a towel to prevent skin damage.
- Apply to the injured area for 20-minute intervals, with breaks in between to prevent frostbite.
- Avoid direct contact with the skin, and monitor for any signs of discomfort or skin changes.
- Timing: Ice application is particularly beneficial in the initial hours and days following the injury or surgery, but it can continue to be used as needed throughout the recovery process.
- Considerations: Patients with certain underlying conditions, such as poor circulation, should consult with healthcare professionals before using ice therapy.
Elevation
- Purpose: Elevating the injured leg above the level of the heart helps reduce blood flow to the area, minimizing swelling and discomfort.
- Method:
- Use pillows or specially designed wedges to support the leg in a comfortable position.
- Try to maintain the elevation as much as possible, especially in the initial recovery phase.
- Monitoring for any discomfort or pressure points is essential to avoid additional complications.
- Timing: Elevation is beneficial both in the acute phase after the injury and postoperatively to aid in recovery.
- Considerations: Care must be taken to support the entire leg, including the knee and ankle, to avoid undue pressure or strain on other joints.
Combining Techniques
- Both ice application and elevation can be used in conjunction with one another and alongside pain medications.
- They can also be part of a broader pain management strategy that might include physical therapy, heat therapy, massage, or other complementary therapies.
Pain management for a broken femur requires a multifaceted approach, and techniques like ice application and elevation offer valuable complementary measures. Utilized properly, they can enhance comfort, reduce the need for medication, and support overall recovery. Collaboration with healthcare providers ensures these techniques are applied safely and effectively based on the individual’s unique needs and circumstances.
Communication with Family and Friends
Keeping family and friends informed and engaged is essential for emotional support.
Medical Treatment and Surgery
Choice of Hospital and Surgeon
Selecting an experienced surgeon and well-equipped hospital is crucial for successful treatment.
Preoperative Procedures
These include medical evaluations and pre-surgical planning to ensure optimal outcomes.
Types of Surgery for Fractures
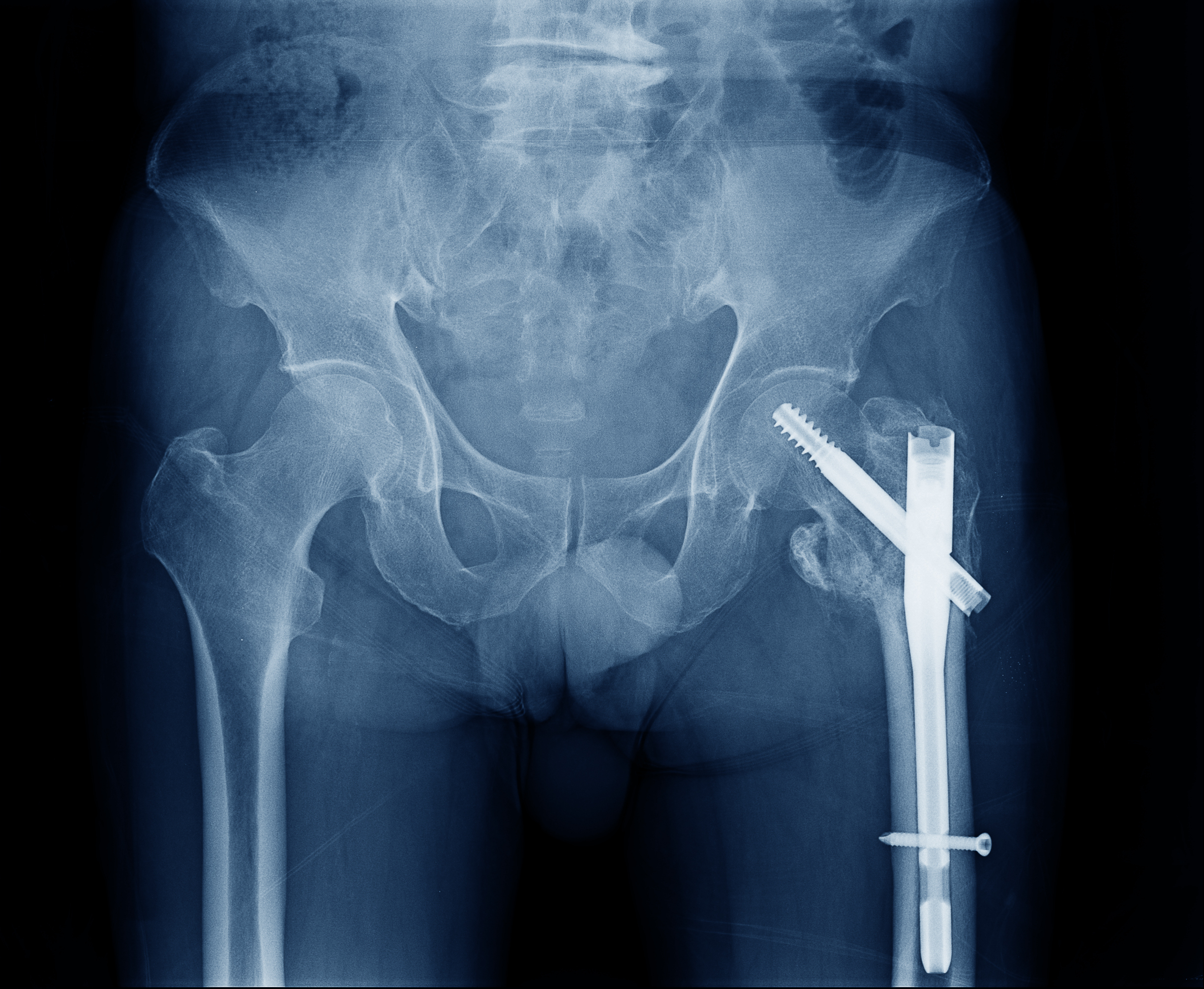
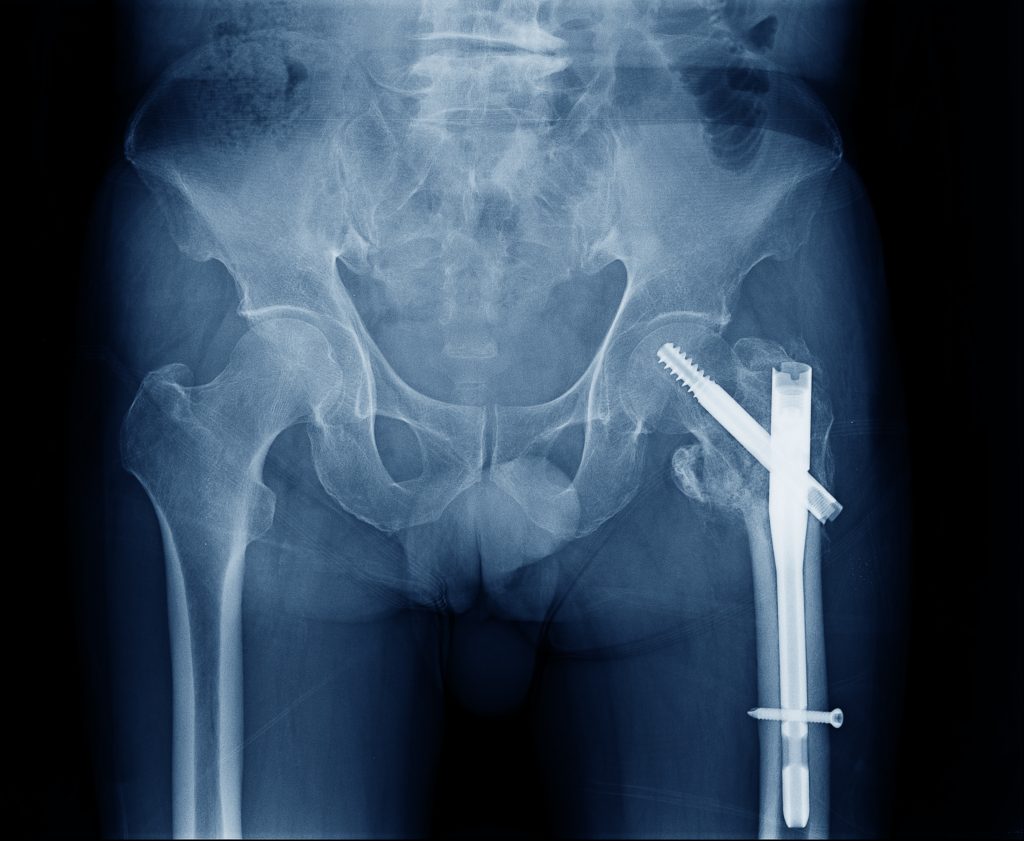
Intramedullary Nailing for Femur Fracture
Purpose
Intramedullary nailing is designed to stabilize and align fractures of the femur by inserting a metal rod (nail) within the marrow canal of the bone. This technique helps in:
- Restoring the alignment and length of the fractured bone.
- Allowing early mobilization and weight-bearing.
- Speeding up the healing process.
Procedure
- Preparation:
- Preoperative planning involves evaluating X-rays and other imaging to determine the appropriate technique and materials.
- The patient is placed under general or spinal anesthesia, and the leg is prepared and draped.
- Accessing the Marrow Canal:
- A small incision is made at the top of the femur, and specialized tools are used to access the marrow canal.
- Inserting the Nail:
- A metal rod, matching the internal diameter of the marrow canal, is carefully inserted into the canal.
- The nail may be hollow or solid and is usually made of titanium or stainless steel.
- Guide wires and reamers may be used to ensure proper alignment and fit.
- Securing the Nail:
- Screws or other locking mechanisms are inserted at the ends of the nail to secure it to the bone, maintaining alignment and allowing the bone to heal around it.
- Closing:
- The incision is closed with sutures or staples, and a dressing is applied.
Benefits
- Provides strong stabilization of the fracture.
- Allows for early movement and weight-bearing, promoting quicker recovery.
- Minimizes the risk of non-union or malunion of the bone.
Potential Risks and Complications
- Infection at the incision site.
- Damage to surrounding tissues or nerves.
- Possible non-union or malunion if not positioned correctly.
- Metal allergies or sensitivities.
Recovery
- Initial recovery involves pain management, wound care, and prevention of blood clots.
- Physical therapy usually begins shortly after surgery to restore mobility and strength.
- Regular follow-ups with the surgeon are necessary to monitor healing through X-rays or other imaging.
- Full recovery can take several months, and the metal rod may remain in place permanently or be removed in a later procedure.
Intramedullary nailing is a sophisticated technique with proven success in the treatment of femur fractures. By understanding the procedure, benefits, and potential risks, patients can engage in informed discussions with their healthcare providers and contribute actively to their recovery process. Collaboration with a skilled surgical team and adherence to postoperative care instructions are crucial for optimal outcomes.
Plates and Screws in Fracture Repair
Purpose
Plates and screws are used to align and hold fractured bone segments in place, allowing them to heal in the correct position. This approach can be used for various types of fractures, including those in the femur, forearm, or other bones.
Procedure
- Preparation:
- Evaluation of the fracture through X-rays and planning the appropriate size and type of plate and screws.
- Anesthesia (either general or regional) and sterilization of the surgical area.
- Exposure and Alignment:
- An incision is made to expose the fracture site.
- The fractured bone segments are realigned to their normal position.
- Placement of Plate:
- A metal plate, usually made of stainless steel or titanium, is placed against the bone along the fracture line.
- The plate is shaped and contoured to match the natural curve of the bone.
- Insertion of Screws:
- Screws are inserted through the holes in the plate and into the bone, anchoring the plate securely.
- The screws’ length and size are carefully selected to ensure proper grip without damaging the bone.
- Closing:
- The incision is sutured, and dressings are applied.
Benefits
- Rigid stabilization allows for early mobilization and can reduce healing time.
- Precise alignment helps in restoring normal function and appearance.
- Adaptable to various types of fractures.
Potential Risks and Complications
- Infection at the surgical site.
- Damage to surrounding nerves or blood vessels.
- Possible loosening or breakage of the plate or screws, requiring revision surgery.
- Temporary or permanent stiffness in the joint near the fracture.
Recovery
- Postoperative care includes pain management, wound monitoring, and early physical therapy.
- A follow-up schedule with the surgeon will include imaging to assess healing progress.
- Rehabilitation will focus on regaining range of motion, strength, and function.
- Plates and screws may remain in place permanently, or removal may be an option depending on individual circumstances.
The use of plates and screws for fracture stabilization is a versatile and effective surgical technique. Careful surgical planning, execution, and postoperative care are vital for successful outcomes. Collaboration with skilled surgeons and adherence to rehabilitation plans ensure optimal healing and return to normal function. Understanding this procedure allows patients to actively participate in their care and recovery process.
External Fixation in Fracture Repair
Purpose
External fixation is employed to stabilize fractures by using pins or screws placed into the broken bone, connected to a stabilizing frame outside the skin. This method is often used for:
- Complex fractures with multiple breaks or comminuted fractures.
- Open fractures with significant skin or soft tissue damage.
- Temporary stabilization before definitive surgery.
- Fractures in infected areas.
Procedure
- Preparation:
- Evaluation through imaging to determine the best placement for pins and screws.
- Administration of anesthesia and preparation of the surgical area.
- Insertion of Pins and Screws:
- Small incisions are made, and pins or screws are inserted into the bone fragments.
- Care is taken to avoid damage to nerves, blood vessels, or other structures.
- Connection to External Frame:
- The pins or screws are connected to a rigid external frame, usually made of metal or carbon fiber rods.
- Adjustments are made to align the bone fragments properly.
- Finalizing the Structure:
- Clamps, rods, and other components are tightened, securing the fractured pieces in the desired position.
- Wound Care:
- The incisions are closed, leaving the part where the pins protrude through the skin open and dressed appropriately.
Benefits
- Allows for easy wound care and inspection, especially in open fractures.
- Adjustable during the healing process without additional surgery.
- Minimizes further damage to soft tissues.
- Can be applied quickly in emergency or trauma situations.
Potential Risks and Complications
- Infection at the pin sites.
- Loosening or migration of pins, affecting fracture alignment.
- Discomfort or irritation from the external frame.
- Potential scarring at the pin sites.
Recovery
- Regular cleaning and care of pin sites to prevent infection.
- Monitoring and adjustments by the surgeon as needed.
- Physical therapy to maintain joint mobility and muscle strength.
- Gradual removal of the external fixator as healing progresses, either in outpatient settings or with minor surgery.
External fixation is a versatile and often lifesaving technique for complex and challenging fractures. Although it may seem more cumbersome compared to internal fixation, its adaptability and the ability to treat certain fractures make it invaluable. Collaboration with an experienced medical team and strict adherence to postoperative care guidelines can lead to successful outcomes. Understanding this procedure can empower patients to actively engage in their recovery and healing journey.
Postoperative Care Following Fracture Repair Surgery
Wound Care
- Inspection and Cleaning:
- Regular inspection of the surgical site for signs of infection, swelling, or other abnormalities.
- Gentle cleaning with prescribed antiseptics or saline solution.
- Instructions may vary depending on the type of surgery (e.g., internal fixation, external fixation).
- Dressing Changes:
- Dressings may need to be changed at regular intervals to keep the wound clean and dry.
- Sterile technique is essential to prevent infection.
- Monitoring for Complications:
- Observing for signs of infection, including increased redness, swelling, warmth, or oozing.
Medication Management
- Pain Control:
- Pain medication, including analgesics or NSAIDs, will be prescribed to manage postoperative discomfort.
- Careful monitoring for side effects and adherence to prescribed dosages.
- Antibiotics:
- If there’s a risk of infection, antibiotics may be prescribed.
- Completion of the entire antibiotic course is vital, even if symptoms improve earlier.
- Anticoagulants:
- To prevent blood clots, especially in patients with limited mobility, anticoagulants might be prescribed.
Early Mobilization and Physical Therapy
- Initial Movement:
- Depending on the type of surgery, gentle movements may be encouraged early to prevent stiffness.
- Guidance from healthcare professionals is crucial to avoid disrupting the surgical site.
- Physical Therapy:
- A tailored physical therapy plan may be implemented to restore strength, flexibility, and function.
- This plan may include passive and active exercises, aquatic therapy, and other specialized techniques.
- Weight-Bearing Guidelines:
- Specific instructions regarding weight-bearing on the affected limb will be provided based on the fracture and repair method.
Ongoing Monitoring and Follow-up Care
- Regular Check-ups:
- Scheduled follow-up appointments with the surgeon or healthcare provider to assess healing progress through physical examination and imaging.
- Adjustments to Treatment:
- Changes to medication, therapy, or other care components based on individual healing progress.
Postoperative care is multifaceted and requires a collaborative effort between healthcare providers and patients. Adherence to wound care, medication protocols, and early mobilization guidelines plays a vital role in achieving successful outcomes. Open communication with healthcare professionals, a clear understanding of the postoperative care plan, and active participation in the healing process can significantly enhance recovery after fracture repair surgery. Patients should always feel empowered to ask questions and seek guidance from their medical team to navigate this essential phase of their recovery journey.
Rehabilitation Plans for Recovery from Fracture Surgery
Importance of a Tailored Rehabilitation Plan
A personalized rehabilitation plan is vital to address the unique needs, goals, and conditions of each patient. A customized approach ensures that therapy is aligned with the specific type and location of the fracture, surgical technique, and individual patient factors like age, occupation, lifestyle, and overall health.
Assessment and Planning
- Initial Evaluation:
- Comprehensive assessment by a physical therapist, including medical history, current mobility, pain levels, and individual goals.
- Collaboration with the surgical team to understand the details of the surgery and any specific restrictions or guidelines.
- Setting Goals:
- Identifying short-term and long-term goals that are realistic and aligned with the patient’s needs and desires.
- This may include returning to specific sports, hobbies, work tasks, or general daily living activities.
- Developing the Plan:
- Designing a rehabilitation program that includes various therapies, exercises, and interventions.
- Regularly reviewing and updating the plan to reflect the patient’s progress and changing needs.
Components of the Rehabilitation Plan
- Physical Therapy:
- Exercises to improve strength, flexibility, balance, and coordination.
- Modalities like ultrasound, electrical stimulation, or heat/cold therapy as needed.
- Occupational Therapy (if applicable):
- Focusing on skills necessary for daily living, work-related tasks, or specific hobbies.
- Pain Management:
- Techniques to control pain, such as medication, relaxation methods, or alternative therapies like acupuncture.
- Education and Support:
- Providing information and training to manage the injury at home, including exercises, precautions, and self-care techniques.
- Emotional and psychological support, including counseling or support groups if needed.
Monitoring Progress
- Regular Evaluations:
- Ongoing assessments to track progress, modify goals, and adjust the plan as needed.
- Collaboration with the surgical and medical team to ensure a unified approach.
- Patient Engagement:
- Encouraging active participation and feedback from the patient.
- Providing education and resources to empower the patient in their recovery.
Long-term Considerations
- Maintenance Programs:
- Continuing exercises or activities that support long-term health and well-being.
- Lifestyle modifications or ergonomic adjustments as needed to prevent future injuries.
Creating a tailored rehabilitation plan is a complex process that requires expertise, collaboration, and active patient participation. The result is a smoother, more effective recovery path that aligns with the individual’s specific needs and goals. Such personalized care fosters a positive healing environment, supports emotional well-being, and maximizes the likelihood of returning to a full and active lifestyle. It’s a critical step in the overall care journey for anyone recovering from a fracture surgery.
Rehabilitation and Physical Therapy
Importance of Rehabilitation in Recovering from a Fracture
Restoration of Function
- Physical Function:
- Rehabilitation aids in regaining strength, flexibility, coordination, and balance.
- Tailored exercises and therapies target specific muscles and joints to restore normal function.
- Enables patients to return to daily activities, work, hobbies, or sports.
- Psychological Function:
- Encourages mental resilience and coping with the emotional challenges of recovery.
- Enhances motivation, self-confidence, and overall well-being.
Promoting Independence
- Self-Care Skills:
- Occupational therapy may teach adaptive techniques for personal care, cooking, or other daily tasks.
- Empowers patients to lead an independent life, even with temporary or permanent limitations.
- Mobility Training:
- Instruction on safe movement, use of assistive devices, or modifications to home and work environments.
- Encourages independent mobility and reduces reliance on caregivers.
Minimizing Complications
- Prevention of Secondary Issues:
- Early and consistent rehabilitation can prevent secondary problems such as joint stiffness, muscle atrophy, or chronic pain.
- Supports overall health by encouraging physical activity and healthy lifestyle habits.
- Monitoring and Management:
- Regular assessments can identify and address potential complications or barriers to recovery.
- Ensures timely intervention if problems arise.
Tailored Approach
- Individualized Care:
- Rehabilitation plans are personalized to the patient’s needs, goals, type of fracture, surgical intervention, and lifestyle.
- Enhances effectiveness and relevance of rehabilitation interventions.
- Interdisciplinary Collaboration:
- Collaboration between medical professionals, including surgeons, physical therapists, occupational therapists, psychologists, and others.
- Ensures a unified approach and continuity of care.
Enhancing Quality of Life
- Holistic Well-being:
- Focuses not only on physical recovery but also emotional, social, and vocational well-being.
- Supports a return to a fulfilling and productive life.
Rehabilitation is more than a series of exercises and therapies; it’s a comprehensive approach to restoring function, promoting independence, minimizing complications, and enhancing quality of life after a fracture. The process is complex and requires expertise, dedication, and active participation from both healthcare providers and patients. It’s an investment in the full spectrum of recovery, encompassing physical, emotional, and social aspects. Recognizing the importance of rehabilitation and engaging in the process can make a profound difference in the outcomes and overall life satisfaction following a fracture. It’s a key step in not only healing from the injury but thriving beyond it.
Choosing a Physical Therapist: A Guide to a Successful Rehabilitation Journey
Understanding the Importance of Selection
- Expertise and Specialization:
- Different therapists may have various specializations, such as sports injuries, orthopedic rehabilitation, or geriatric care.
- Selecting a therapist with experience in treating fractures or the specific type of injury can greatly enhance the effectiveness of therapy.
- Personalized Care:
- A skilled therapist can develop a tailored rehabilitation plan, considering factors like age, occupation, lifestyle, and individual goals.
- This personalization ensures that therapy is targeted and relevant to the patient’s unique needs.
Key Factors to Consider
- Qualifications and Licensing:
- Check for proper educational credentials, licensing, and certifications.
- Special certifications may indicate additional training or expertise in a particular area.
- Experience and Track Record:
- Consider the therapist’s experience with similar injuries or surgeries.
- Asking for patient testimonials or reading reviews can provide insights into others’ experiences.
- Treatment Philosophy and Approach:
- Understanding the therapist’s approach to care, including their beliefs about patient involvement, use of manual therapy, exercise prescription, etc.
- Ensuring that their philosophy aligns with your expectations and preferences.
- Location and Accessibility:
- Proximity to home or work may be important, especially with frequent appointments.
- Consider accessibility factors like parking, public transportation, or the facility’s ability to accommodate any special needs.
- Insurance and Financial Considerations:
- Verify that the therapist accepts your insurance or understand any out-of-pocket costs.
- Discussing payment options and potential financial assistance if needed.
Strategies for Selection
- Ask for Recommendations:
- Consult with your healthcare provider, surgeon, or friends and family who may have experienced similar rehabilitation.
- They may provide trusted recommendations based on personal experiences or professional knowledge.
- Interview Potential Therapists:
- Schedule a consultation or interview with potential therapists.
- This provides an opportunity to ask questions, understand their approach, and assess compatibility.
- Visit the Facility:
- Touring the therapy facility can give you a sense of the environment, equipment, staff, and overall vibe.
- Consider cleanliness, state-of-the-art equipment, and a friendly and professional atmosphere.
Choosing the right physical therapist is a multifaceted decision that requires careful consideration of various factors, from qualifications and experience to personal compatibility and financial considerations. Making an informed choice can set the stage for a targeted, effective, and satisfying rehabilitation process. It’s a partnership that goes beyond exercises and treatments; it’s a collaboration that supports healing, growth, and the return to a fulfilling life after an injury or surgery. Your choice of a physical therapist can be a pivotal part of that journey, so invest time and effort in making the right selection.
Stages of Recovery Following Fracture Repair
Healing Stage
- Immediate Healing (Inflammatory Phase):
- Begins immediately after surgery or injury.
- Focus on controlling swelling, pain, and preventing infection.
- Limited mobility to allow the bone and surrounding tissues to begin the healing process.
- Bone Formation (Repair Phase):
- Gradual rebuilding of bone through callus formation, which may last several weeks.
- Gentle exercises may be introduced to prevent stiffness without disrupting healing.
Strengthening Stage
- Early Strengthening:
- Initiated once sufficient healing is observed.
- Gradual introduction of exercises to build strength in muscles surrounding the fracture site.
- Continued monitoring to avoid overstrain or re-injury.
- Progressive Strengthening:
- Increase in exercise intensity and complexity.
- May include weight-bearing exercises, resistance training, and specialized equipment.
- Collaboration with physical therapists to ensure proper technique and progression.
Functional Restoration Stage
- Restoring Range of Motion:
- Focus on regaining full mobility in the affected limb.
- Use of stretching, mobility exercises, and possibly manual therapy.
- Activity-Specific Training:
- Tailored exercises and activities to match the patient’s lifestyle, occupation, or hobbies.
- Gradual reintroduction to sports, work tasks, or daily activities.
- Balance and Coordination Training:
- Activities to restore proprioception, balance, and coordination.
- Essential for full functional recovery and prevention of future injuries.
Long-term Maintenance and Prevention Stage
- Ongoing Fitness and Well-being:
- Continuation of exercises or activities that support long-term health.
- Regular check-ups with healthcare providers to monitor overall bone health.
- Injury Prevention:
- Education on proper techniques, ergonomics, or lifestyle modifications to prevent re-injury.
- May include recommendations on diet, supplementation, or other wellness practices.
Recovery from a fracture progresses through carefully coordinated stages, from initial healing to full functional restoration. Each stage is essential and builds on the previous one, requiring expert guidance, patient commitment, and time. Understanding these stages can help patients and their support teams navigate the recovery process more effectively, set realistic expectations, and work towards regaining full strength, mobility, and function. It also underscores the importance of a multidisciplinary approach, involving surgeons, physical therapists, occupational therapists, and other healthcare professionals, to ensure a successful recovery.
Exercises and Techniques
Specific exercises and techniques promote flexibility and strength.
Mental Health Support: A Pillar of Holistic Well-being
Mental health is an integral aspect of an individual’s overall health and well-being. It is just as crucial as physical health, but unfortunately, it often does not receive the same attention or priority. Yet, mental and emotional well-being influences everything from our thoughts and feelings to how we cope with stress, relate to others, and make choices.
The Significance of Addressing Mental Health
- Overall Recovery: Mental health conditions, if left untreated, can affect one’s daily life, physical health, and can even lead to chronic medical conditions. Addressing mental health is essential for overall recovery from both emotional and physical trauma.
- Promotion of Healthy Relationships: Good mental health can foster better relationships with family, friends, and colleagues. People with sound mental health are more likely to be understanding, patient, and supportive in their relationships.
- Improved Productivity: Individuals who receive support for their mental health challenges tend to have better focus, resilience, and a higher capacity to handle pressures, resulting in improved productivity at work or school.
Counseling as a Vital Tool
Counseling plays a pivotal role in supporting those with mental health challenges. It offers a safe environment for individuals to express their feelings, understand their conditions, and learn coping mechanisms.
- Self-awareness and Insight: Counseling can help individuals gain insight into their behavior, feelings, and responses to certain situations. This understanding is crucial for personal growth and development.
- Skill Development: Through counseling, individuals can learn essential life skills, such as stress management, problem-solving, and conflict resolution.
- Stigma Reduction: By encouraging the practice of seeking counseling, we can contribute to reducing the stigma associated with mental health. Accepting counseling as a regular part of health care can lead to more people seeking help when they need it.
Mental health support, including counseling, is not just beneficial but necessary for holistic health and well-being. As a society, recognizing and prioritizing mental health will pave the way for happier, more fulfilled lives for countless individuals.
Long-term Prognosis: The Importance of Continuous Follow-up
In the context of mental and physical health, long-term prognosis refers to the likely course and outcome of a condition over an extended period. Continuous follow-up plays a crucial role in ensuring that the long-term prognosis is favorable, as it allows for consistent monitoring, support, and adjustments to treatment plans. Here’s why this continuous care is vital for success:
Monitoring Progress and Making Adjustments
- Identifying Changes: Continuous follow-up allows healthcare providers to identify any changes in a patient’s condition early. This includes both positive progress and potential setbacks or complications.
- Personalized Care: As a patient progresses, the treatment plan may need to be adjusted. Continuous follow-up ensures that the care remains tailored to the individual’s specific needs and circumstances.
- Prevention of Relapse: Regular appointments and check-ups can prevent or catch relapses in conditions early, leading to quicker intervention and avoiding long-term damage or distress.
Addressing Lingering Issues
- Emotional Support: Chronic conditions often come with lingering emotional or psychological issues. Continuous follow-up provides ongoing emotional support, which may include therapy or counseling.
- Managing Chronic Symptoms: Some conditions may leave patients with chronic symptoms that need to be managed over the long term. Regular check-ups ensure that these symptoms are controlled and that the patient’s quality of life is maintained.
Encouraging Compliance and Empowerment
- Enhancing Adherence to Treatment: Continuous follow-up helps ensure that patients adhere to their treatment plans, including taking prescribed medications and following lifestyle recommendations.
- Patient Empowerment: Regular contact with healthcare providers empowers patients with knowledge and support, enabling them to take an active role in their recovery and maintain their health.
Building Trust and Collaboration
- Strengthening Patient-Provider Relationship: Trust is built through consistency and ongoing communication, fostering a collaborative relationship between the patient and the healthcare provider.
- Interdisciplinary Coordination: Long-term care often involves multiple healthcare professionals. Continuous follow-up ensures that all members of the care team are aligned and working towards the same goals.
The long-term prognosis of any medical or mental health condition is not only about initial treatment but continuous, patient-centered follow-up care. This ongoing support ensures that individualized treatment plans are consistently implemented, progress is monitored, and any lingering or emerging issues are addressed promptly. Ultimately, continuous follow-up fosters a comprehensive approach to healthcare, emphasizing prevention, intervention, empowerment, and collaboration, all of which contribute to long-term success and well-being.
Legal Considerations
Legal matters, whether they relate to business, personal affairs, or disputes, often involve intricate rules and regulations that can be difficult for the average person to navigate. Engaging a specialized lawyer early in the process can be crucial in addressing these complexities. Here’s why consulting a legal professional is essential:
Understanding Legal Language and Norms
- Deciphering Legal Jargon: Legal documents and laws are often written in a complex language that can be challenging to interpret. Lawyers are trained to understand this language, ensuring that you fully grasp what’s required or expected.
- Compliance with Legal Procedures: The legal system has specific procedures that must be followed. A lawyer can guide you through these processes, ensuring that all necessary steps are taken correctly and in a timely manner.
Specialization in Different Fields of Law
- Expertise in Relevant Areas: Different legal issues require different expertise. For instance, a family lawyer specializes in matters like divorce and custody, while a corporate lawyer focuses on business-related issues. Engaging a specialized lawyer ensures you receive the most relevant and knowledgeable guidance.
- Staying Up-to-Date: Laws and regulations can change frequently. A specialized lawyer will be aware of the latest developments in their field, providing advice that’s current and applicable.
Strategic Planning and Negotiation
- Developing a Legal Strategy: A lawyer can help you understand the best course of action for your particular situation, considering all the legal angles and potential outcomes.
- Skilled Negotiation: In cases involving settlements or agreements, a lawyer’s negotiation skills can be invaluable in reaching a favorable outcome.
Protection of Rights and Interests
- Advocacy: Lawyers act as your advocates, representing your interests in legal proceedings, negotiations, or disputes.
- Confidentiality: Attorney-client privilege ensures that the information you share with your lawyer is confidential, providing a secure environment to discuss your case openly.
Cost and Time Efficiency
- Avoiding Common Mistakes: Mistakes in legal matters can be costly and time-consuming. Engaging a lawyer early helps prevent these mistakes, saving both time and money.
- Resource Allocation: A specialized lawyer will know how to efficiently allocate resources to various aspects of your case, avoiding unnecessary expenses.
Consulting a lawyer is not simply a formality in the legal process; it’s a strategic move that provides direction, clarity, protection, and efficiency. Engaging a specialized lawyer early in any legal matter ensures that you are guided by expertise tailored to your specific situation. This guidance helps in navigating the legal maze with confidence, ensuring that your rights are protected, your interests are represented, and the best possible outcome is achieved. Whether it’s a personal legal matter or a complex business negotiation, the value of expert legal counsel cannot be overstated.
Understanding Your Right
Knowing your legal rights is not just about having a theoretical grasp of the law; it’s about understanding how those rights apply to your personal or professional life, especially when it comes to claiming fair compensation. Whether you’re dealing with employment disputes, personal injuries, consumer rights, or any other legal matter, a solid understanding of your rights is crucial. Here’s a comprehensive look at why this is essential and how you can make it work for you:
What Are Your Rights?
- Constitutional Rights: These are the basic rights and freedoms guaranteed to individuals by a country’s constitution, including rights like free speech and due process.
- Statutory Rights: These are rights protected by specific laws or regulations, such as labor laws, consumer protection laws, or health and safety regulations.
- Contractual Rights: These rights are agreed upon between parties in a contract, such as an employment contract or purchase agreement.
Importance of Understanding Your Rights in Various Situations
- Employment: Knowing your rights in the workplace, such as rights to fair pay, safe working conditions, and protection against discrimination, enables you to recognize and challenge unfair practices.
- Personal Injury: If you’re injured due to someone else’s negligence, understanding your rights to compensation for medical expenses, lost wages, and other damages is vital.
- Consumer Transactions: Recognizing your rights as a consumer helps you know what to expect from products or services and what to do if those expectations are not met.
How to Understand and Exercise Your Rights
- Educate Yourself: Use reliable sources like government websites, legal guides, and educational institutions to understand your rights in specific situations.
- Consult a Lawyer: If you’re unsure about your rights or how to exercise them, seeking professional legal advice can provide clarity and guidance.
- Document Everything: Keeping thorough records of relevant information, communications, and actions can be essential if you need to prove your case.
- Act Promptly: Many legal rights have time limits for action, so it’s important to act quickly if you believe your rights have been violated.
Challenges and Pitfalls to Avoid
- Relying on Misinformation: Not all information online or from peers is accurate. Ensuring you consult credible sources or professionals helps avoid misunderstandings.
- Failing to Act: Knowing your rights is only the first step; you must also be willing to assert them. Failure to act may lead to loss of rights or remedies.
Understanding your legal rights is a fundamental aspect of empowered citizenship. It helps you navigate complex legal landscapes, make informed decisions, and protect your interests, particularly when it comes to claiming fair compensation.
Whether you’re dealing with a personal injury claim, a workplace issue, or a consumer dispute, the process begins with knowing what your rights are and how to assert them effectively. Investing time in educating yourself, consulting with professionals when needed, and being proactive in exercising your rights can lead to a more just and favorable outcome. It puts you in a position of strength, enabling you to claim the fair compensation to which you’re entitled, and ensures that your voice is heard in situations where it matters most.
Compensation and Insurance Claims
Dealing with insurance policies and compensation claims can be a complex and daunting process. Whether following an accident, illness, property damage, or other loss, understanding the mechanisms involved is vital to securing the financial support necessary for recovery. Below are key aspects to consider when dealing with compensation and insurance claims:
Understanding Insurance Policies
- Know Your Coverage: Different insurance policies cover various aspects. Understanding what is included in your coverage and any limitations or exclusions is essential for filing a successful claim.
- Reading the Fine Print: Insurance policies often contain complex terms and conditions. Carefully reading and understanding these terms ensures that you are aware of your entitlements and obligations.
- Consulting with an Insurance Agent or Broker: Professionals in the insurance field can clarify uncertainties and guide you in understanding your policy.
Navigating Compensation Claims
- Immediate Reporting: Promptly reporting the incident to the insurance company is often required. Delay can lead to denial or complications in processing the claim.
- Gathering Evidence: Collecting evidence like photographs, witness statements, police reports, and medical records can support your claim.
- Seeking Legal Advice: In some cases, consulting a lawyer specializing in compensation and insurance law can be beneficial in understanding your rights and guiding you through the process.
Dealing with Different Types of Claims
- Health Insurance Claims: These may include medical bills, prescriptions, and therapies. Understanding the network of providers and pre-authorization requirements is essential.
- Auto Insurance Claims: You may be entitled to compensation for vehicle repairs, rental cars, medical expenses, and more, depending on the policy and circumstances.
- Property Insurance Claims: These claims deal with damage to or loss of property. Knowing the type of coverage, such as replacement cost or actual cash value, is vital.
Negotiating Settlements
- Fair Assessment: It’s important to evaluate the offer from the insurance company to ensure that it accurately reflects the loss or damages incurred.
- Negotiation Skills: You may need to negotiate with the insurance adjuster. Understanding your policy and having proper documentation will strengthen your position.
Avoiding Common Pitfalls
- Claims often have specific time limits for filing. Missing these deadlines can lead to a denial of the claim.
- Complete Documentation: Incomplete or inaccurate information can delay or jeopardize the claim. Ensuring all required documentation is provided is crucial.
Understanding insurance policies and compensation avenues is not merely about reading a document; it involves a comprehensive approach to knowing your rights, obligations, and the nuances of the claim process. From understanding different coverages to knowing how to negotiate and what evidence to gather, the process requires diligence and sometimes professional guidance.
Securing financial support through compensation and insurance claims is a fundamental aspect of recovery and rebuilding. It provides the monetary means to address medical needs, property repairs, or other losses. By actively engaging with the process and seeking professional help when needed, individuals can navigate the complexities of insurance claims and obtain the financial support they are entitled to.
Femur injuries can have life-altering consequences, leading to substantial medical expenses, loss of income, and prolonged physical suffering. We recognize the complexity and emotional toll of these cases, and we’re committed to fighting for the rights and fair compensation of those affected. With a team of experienced and compassionate legal professionals, we stand ready to guide you through every step of the legal process, providing personalized attention and unwavering advocacy. If you or a loved one has suffered a femur injury due to someone else’s negligence, don’t hesitate to contact us for a free consultation. Together, we’ll work to ensure that justice is served, and your future is secured.